BACKGROUND
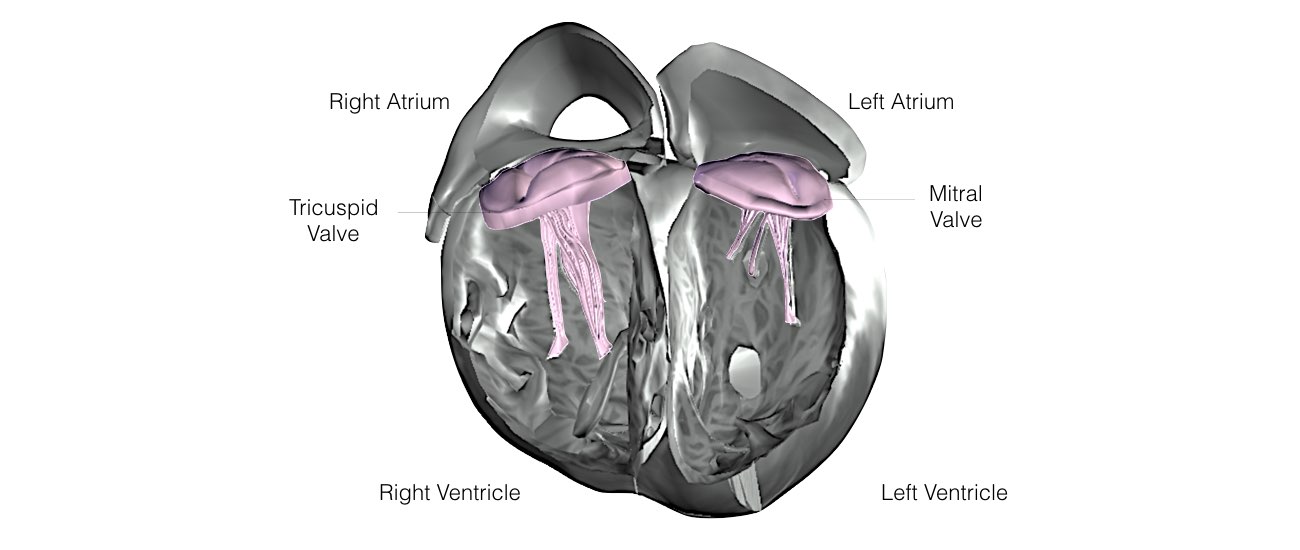
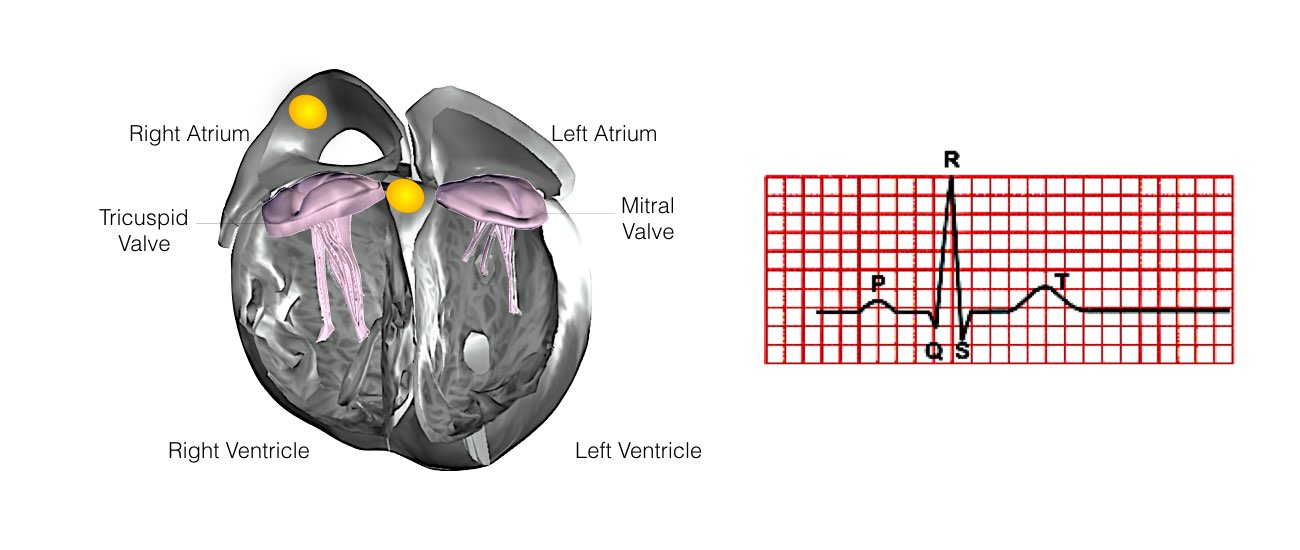
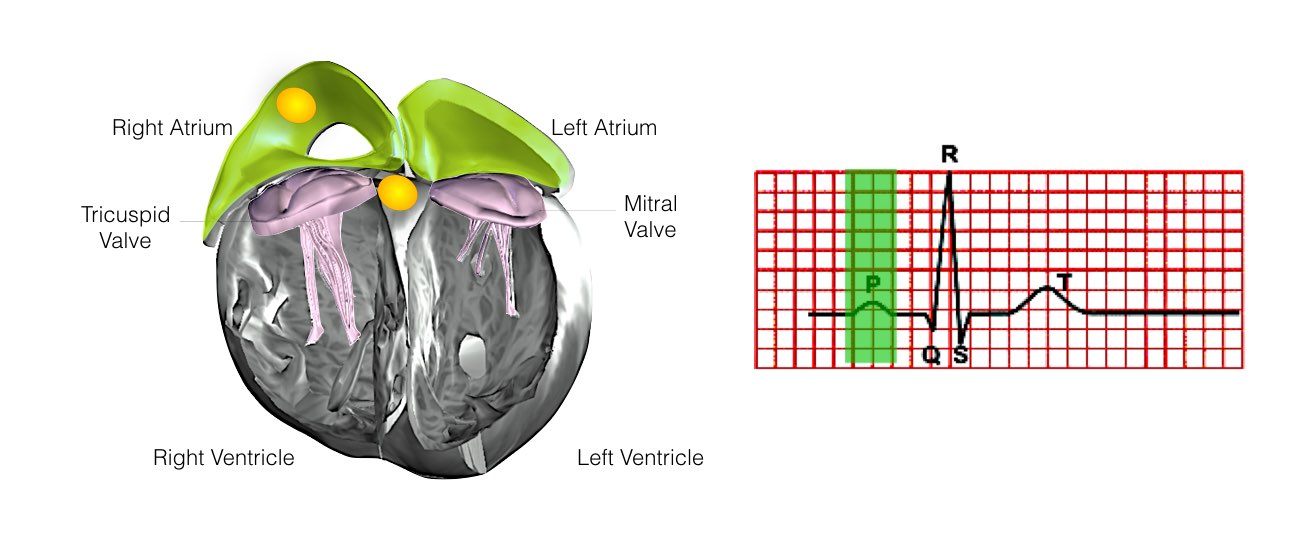
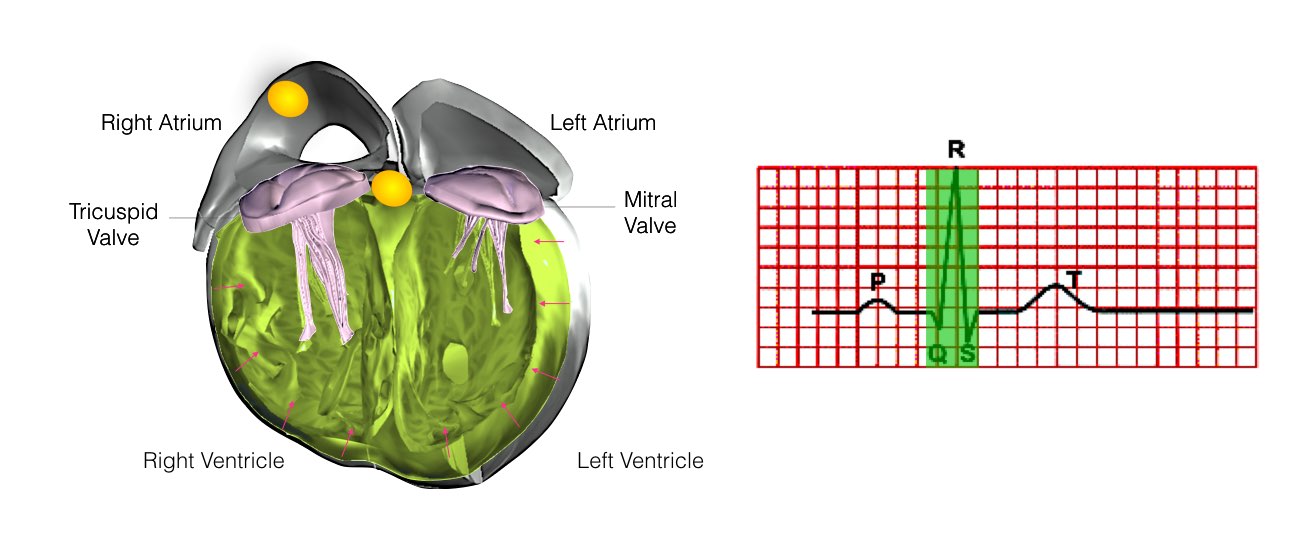
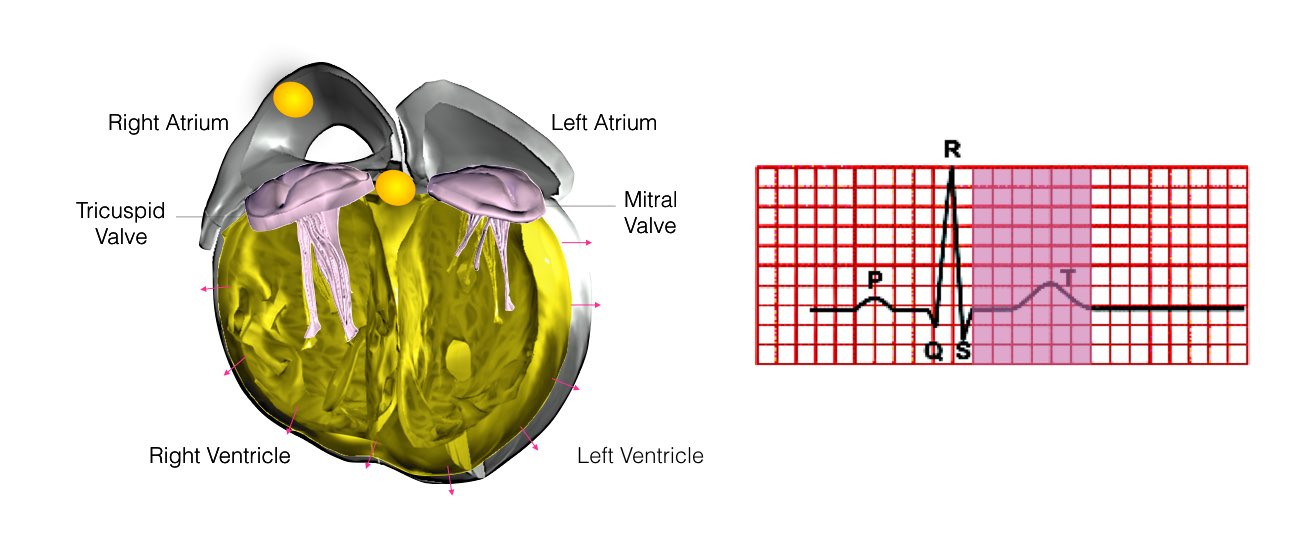
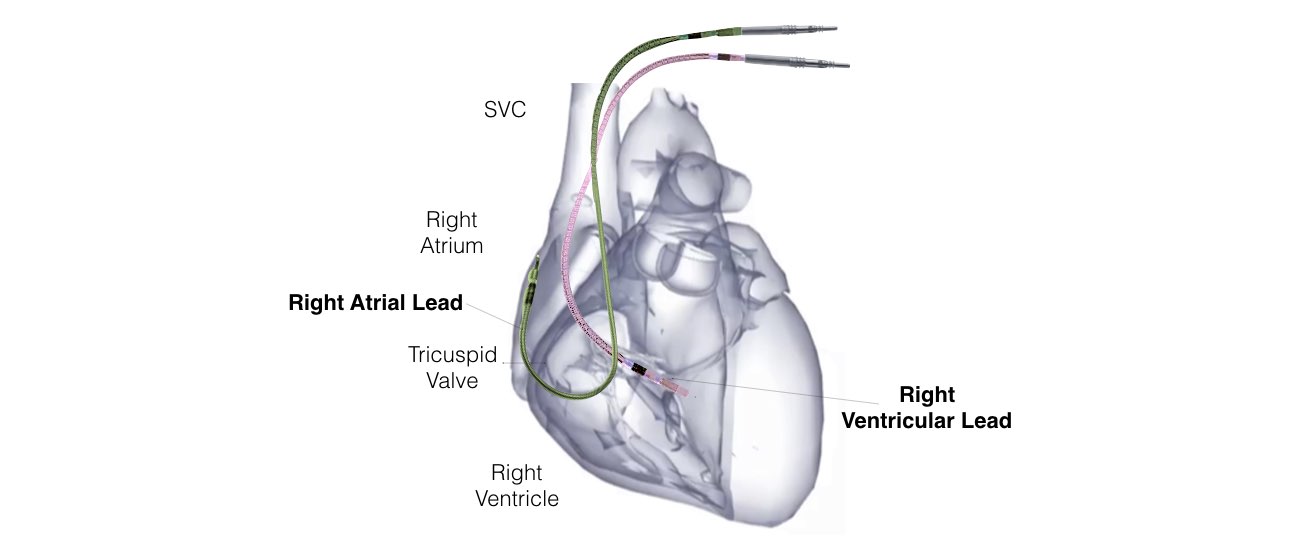
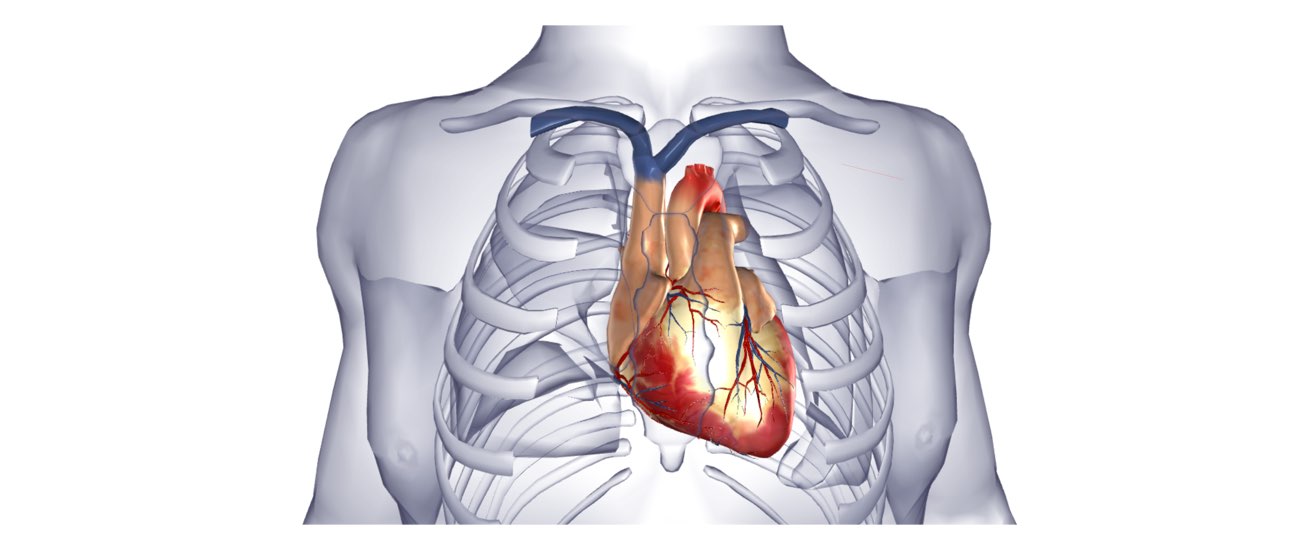
The heart is a pump responsible for maintaining blood supply to the body. It has four chambers. The two upper chambers (the right atrium and left atrium) are the chambers that receive blood as it returns from the body via the veins. The lower chambers (the right and left ventricle) are the chambers responsible for pumping the blood out to the body via the arteries. Like any pump, the heart has an electrical system that controls how it functions.
Normal heart rhythm.
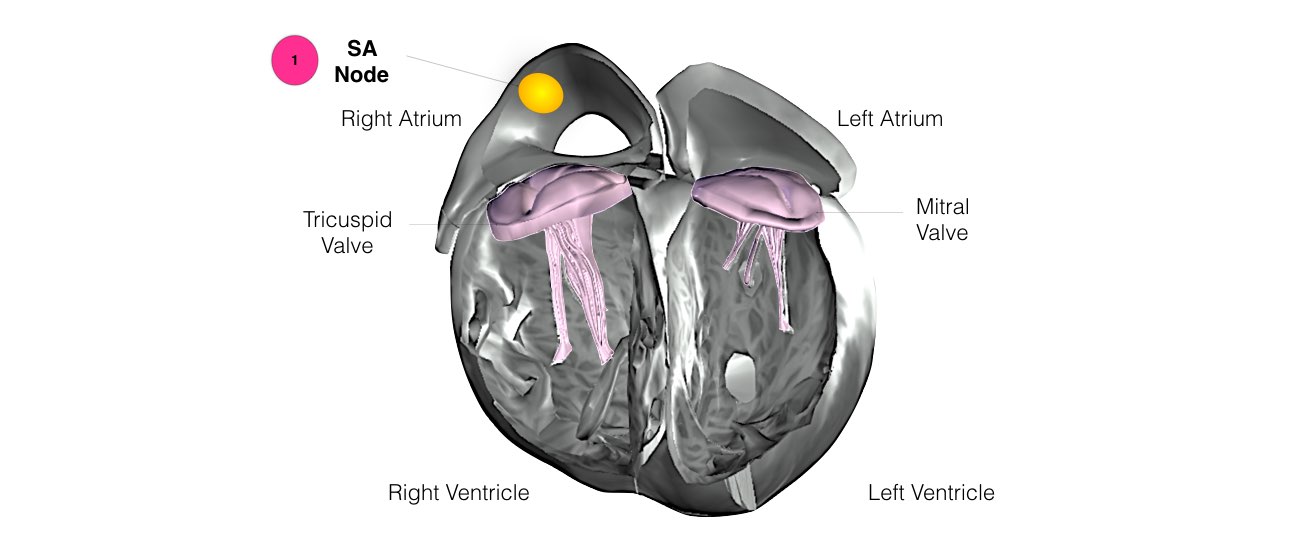
In order for the heart to do its work (pumping blood throughout the body), it needs a sort of spark plug or electrical impulse to generate a heartbeat. Normally this electrical impulse begins in the upper right chamber of the heart (in the right atrium) in a place called the sino-atrial (SA) node. The SA node is the natural pacemaker of the heart. The SA node gives off electrical impulses to generate a heartbeat in the range of 60 to 100 times per minute. If you are exercising, doing strenuous work or are under stress, your heart rate will be faster. When you rest or sleep your heart rate will slow down. If you take certain medications, your heart rate may be slower.
From the Sinus Node, the electrical impulse is relayed along the heart’s conduction system. It spreads throughout both the right and left atria causing them to contract evenly.
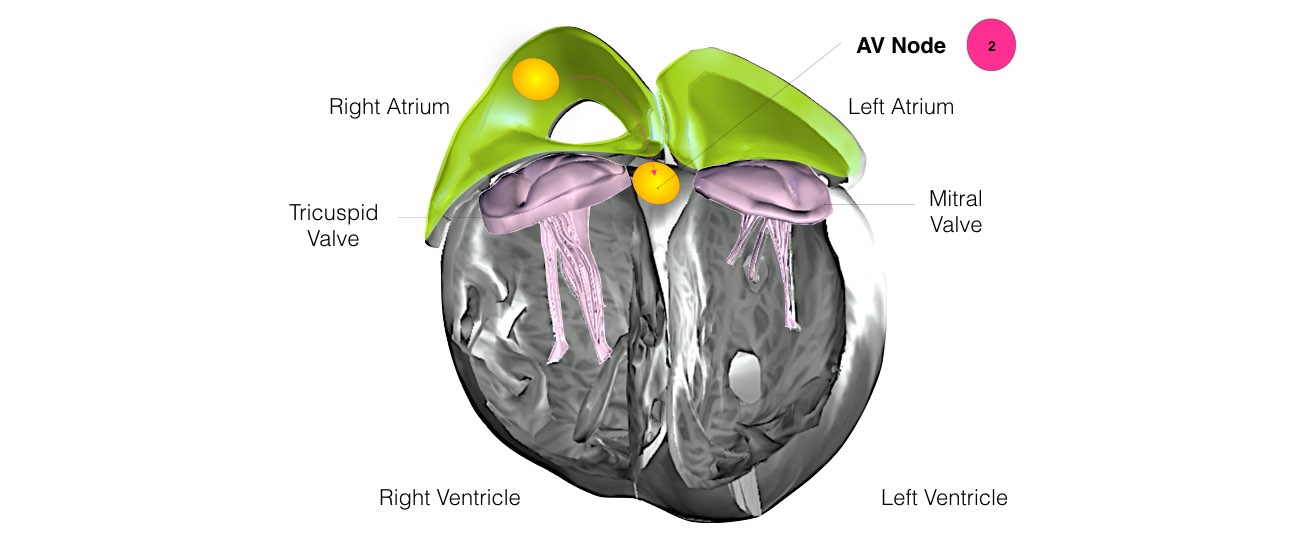
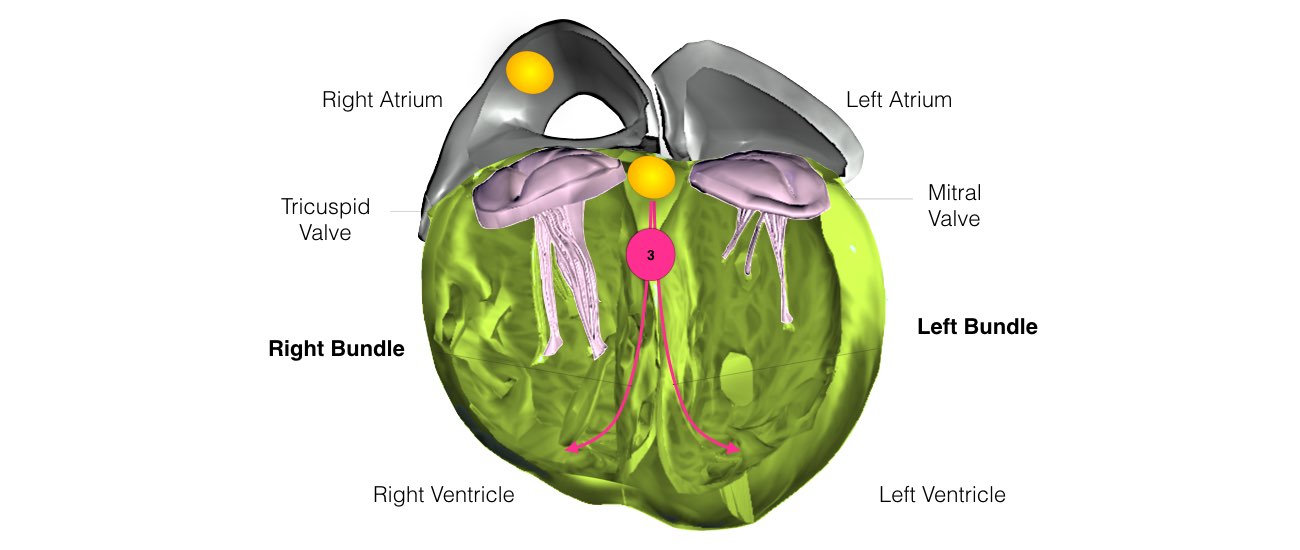
When the impulse spreads over the right atrium it reaches the atrio-ventricular (AV) node. This is a very important structure in the heart because it is the only electrical connection between the top chambers and the bottom chambers. It is therefore the only way in which an electrical impulse can reach the pumping chambers (the ventricles). The impulse spreads through the AV node and down into the lower chambers or ventricles of the heart. This causes them to contract and pump blood to the lungs and body.
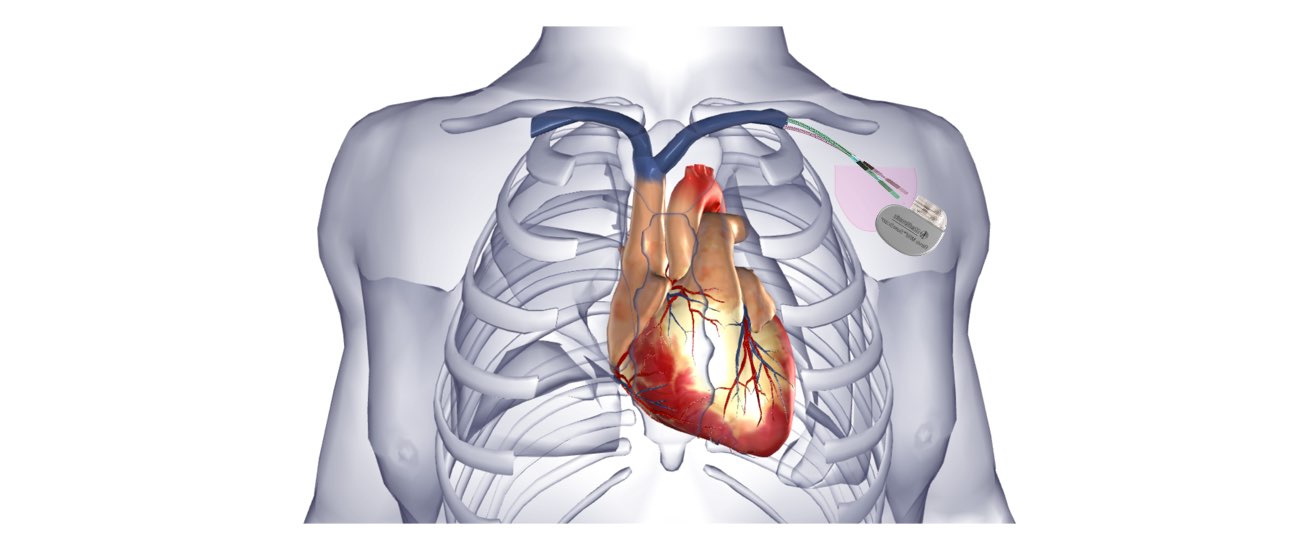
Why do I need a pacemaker?
In some people the electrical system of the heart may stop working properly. This can occur in a number of different ways. Sometimes the SA node fails to make enough impulses and the heart slows down and even pauses. This is sometimes called “sick sinus syndrome”. On other occasions, even though the SA node is making enough impulses, there are problems with either the AV Node, or the left and right bundle branches. When this happens, the impulses are not conducted down into the pumping chambers. This is termed “heart block” (This doesn’t mean there are blockages in arteries but rather in the electrical system). This will also cause the heart to slow down or pause.
What symptoms will I experience?
When the heart slows down or pauses symptoms may include tiredness, breathlessness or lightheadedness.
However, commonly when the heart pauses, you will experience dizziness or actually pass out and collapse. You may experience very little or no warning prior to collapsing