BACKGROUND
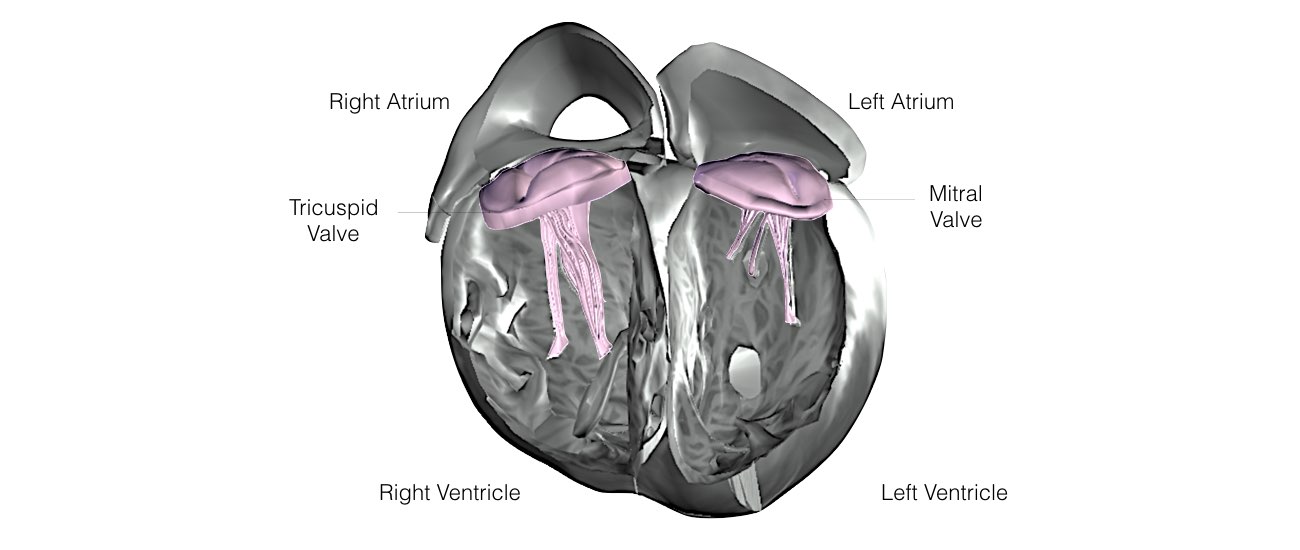
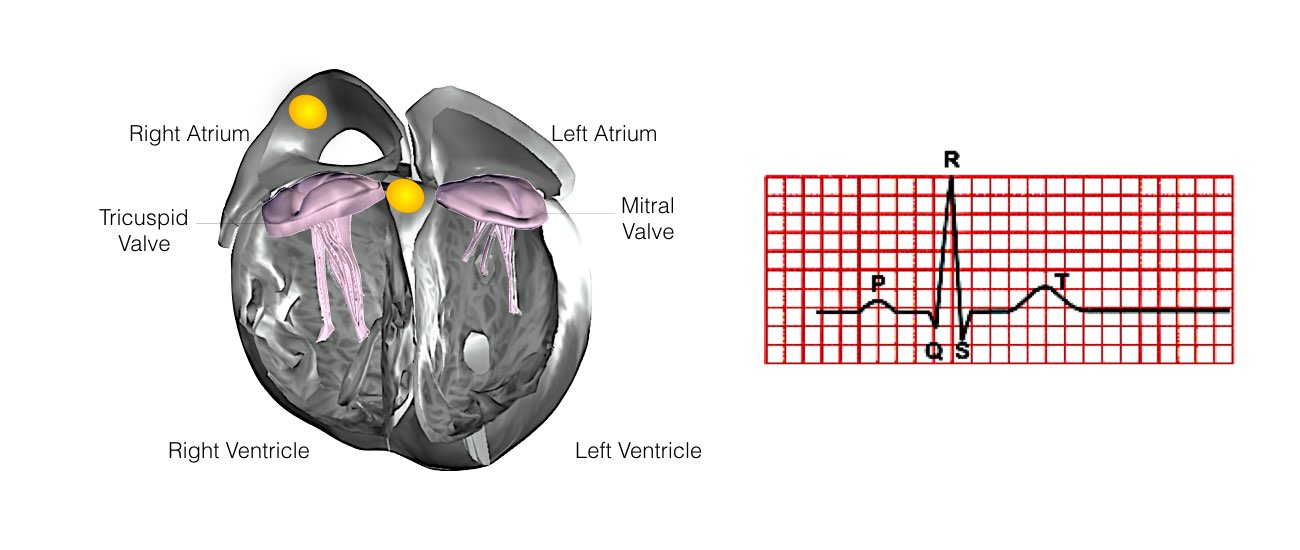
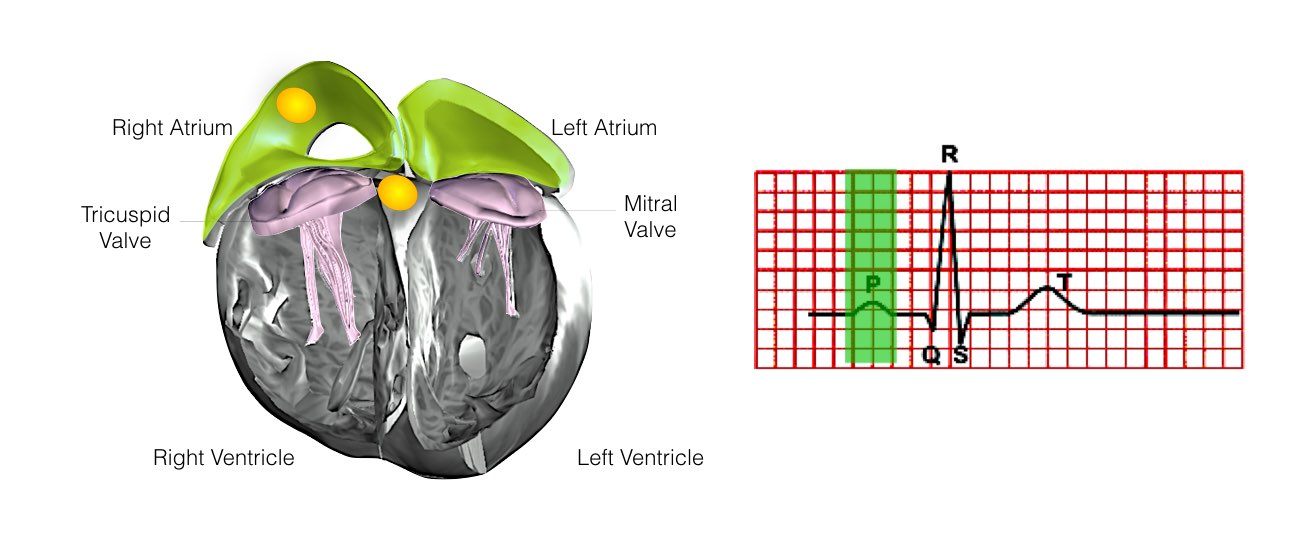
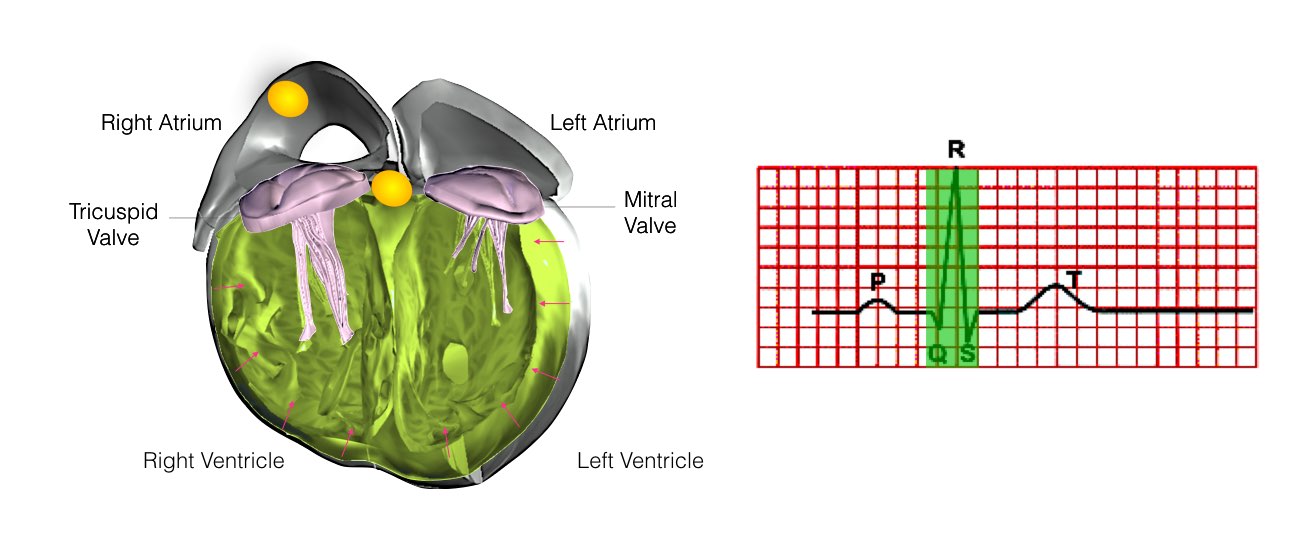
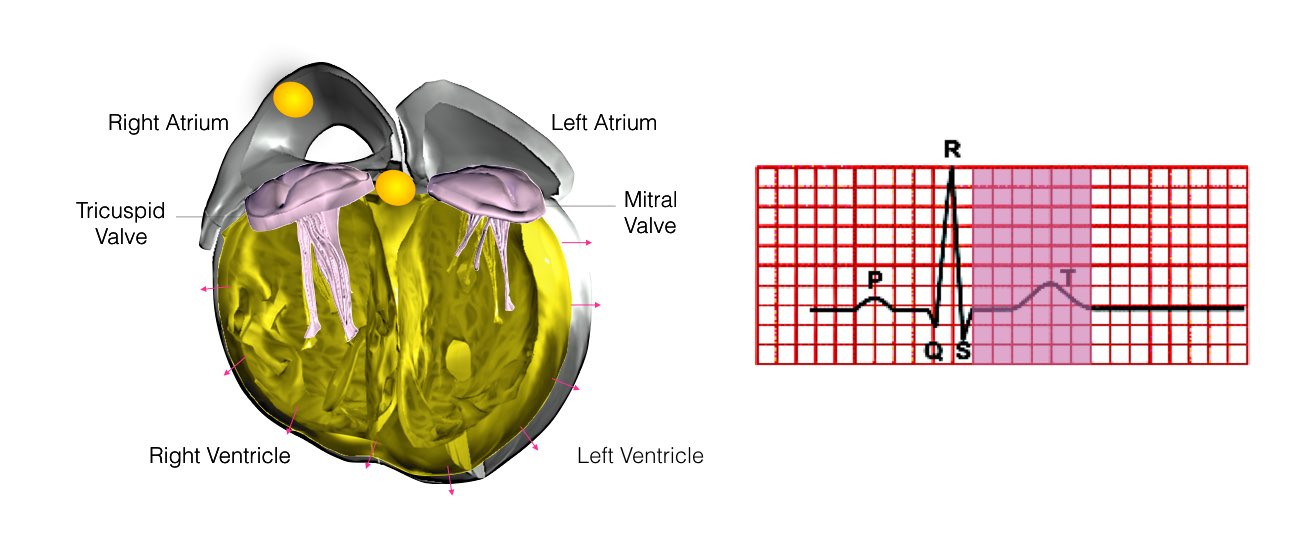
The heart is a pump responsible for maintaining blood supply to the body. It has four chambers. The two upper chambers (the right atrium and left atrium) are the chambers that receive blood as it returns from the body via the veins. The lower chambers (the right and left ventricle) are the chambers responsible for pumping the blood out to the body via the arteries. Like any pump, the heart has an electrical system that controls how it functions.
Normal heart rhythm.
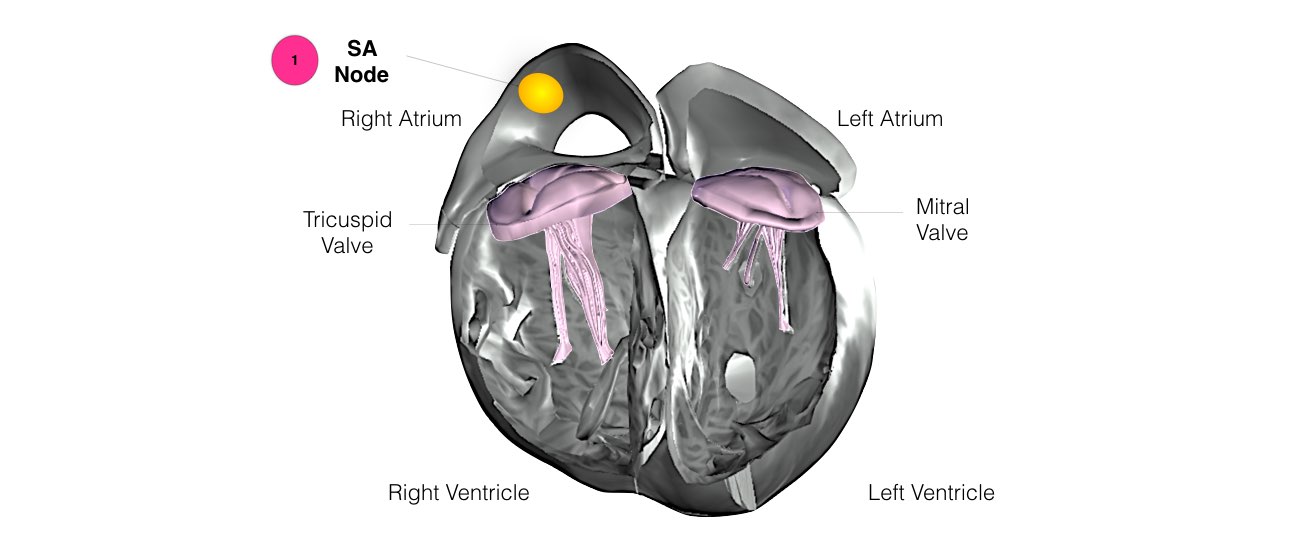
In order for the heart to do its work (pumping blood throughout the body), it needs a sort of spark plug or electrical impulse to generate a heartbeat. Normally this electrical impulse begins in the upper right chamber of the heart (in the right atrium) in a place called the sino-atrial (SA) node. The SA node is the natural pacemaker of the heart. The SA node gives off electrical impulses to generate a heartbeat in the range of 60 to 100 times per minute. If you are exercising, doing strenuous work or are under stress, your heart rate will be faster. When you rest or sleep your heart rate will slow down. If you take certain medications, your heart rate may be slower.
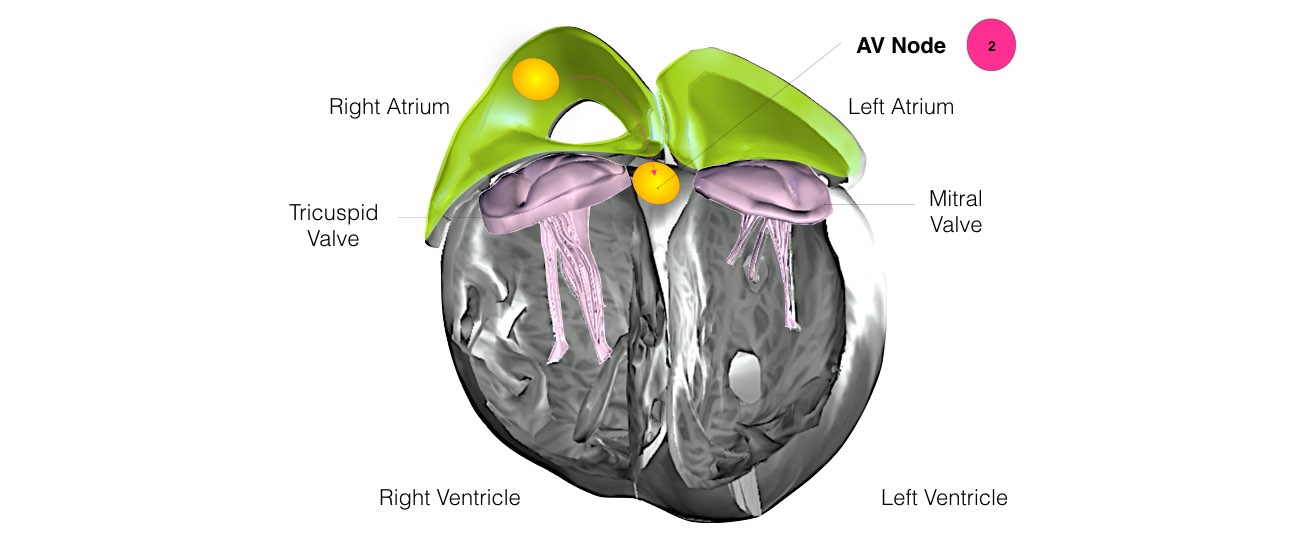
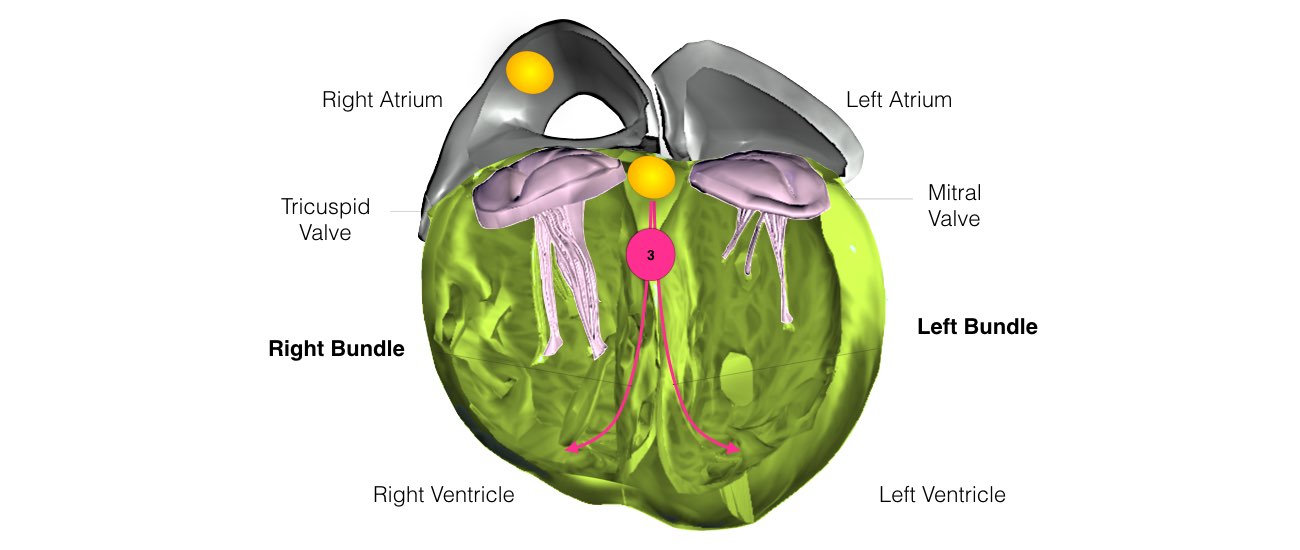
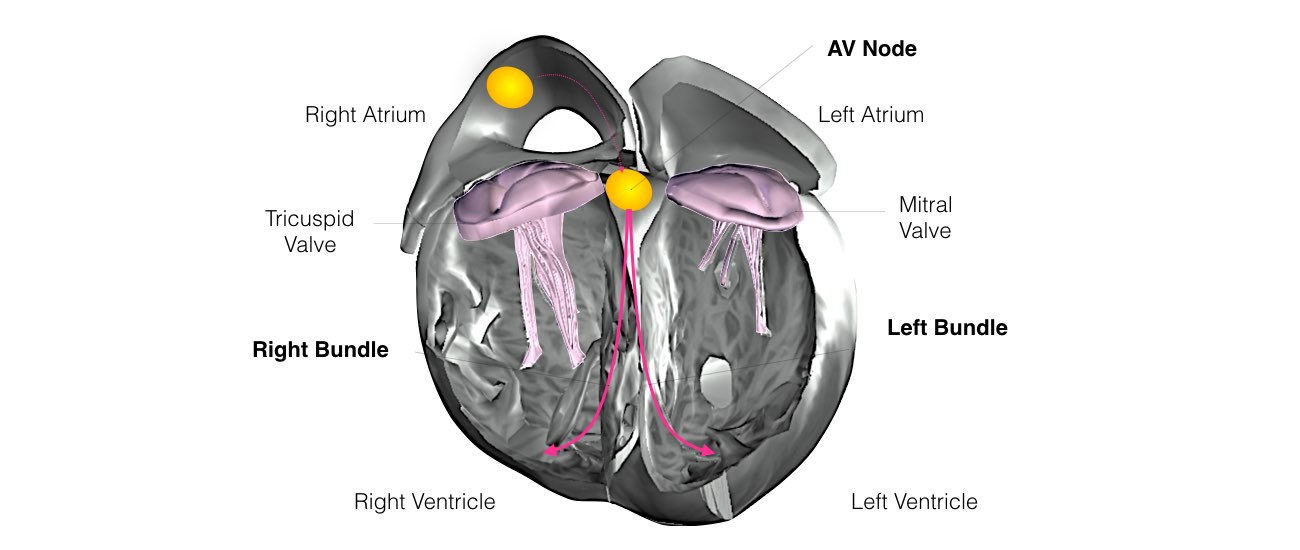
From the Sinus Node, the electrical impulse is relayed along the heart’s conduction system. It spreads throughout both the right and left atria causing them to contract evenly.
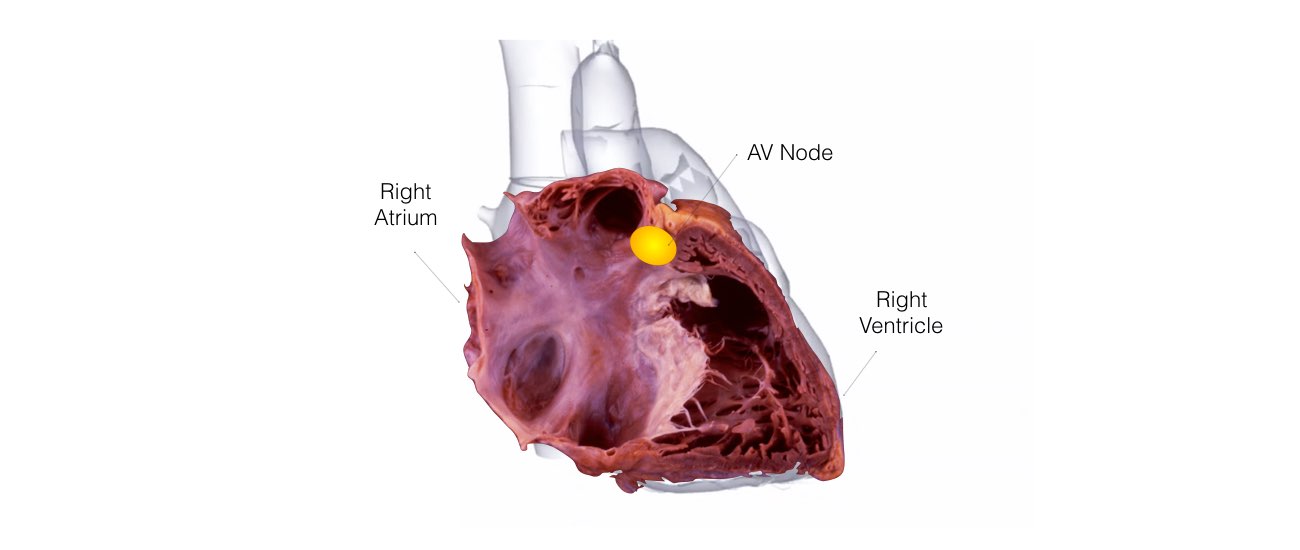
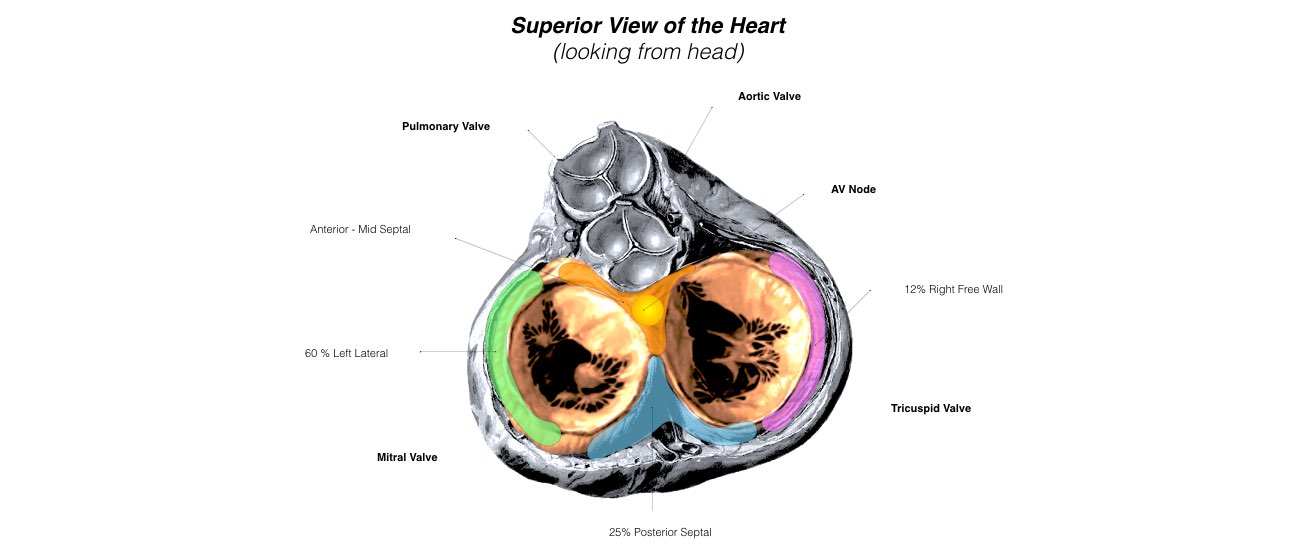
When the impulse spreads over the right atrium it reaches the atrio-ventricular (AV) node. This is a very important structure in the heart because it is the only electrical connection between the top chambers and the bottom chambers. It is therefore the only way in which an electrical impulse can reach the pumping chambers (the ventricles). The impulse spreads through the AV node and down into the lower chambers or ventricles of the heart. This causes them to contract and pump blood to the lungs and body.
What is Supraventricular tachycardia?
In some hearts, an abnormal heart rhythm develops in the top part of the heart when an electrical impulse either starts from a different location other than the SA node, or follows a route (or pathway) that is not normally present. When this occurs the heart will suddenly start racing. The heart rate is usually over 150 beats per minute and often over 200 beats per minute. Certain things in some people can trigger episodes. These include caffeine, alcohol, anxiety, exercise or sudden movements such as bending over. However, often these episodes can occur at any time without a trigger. During an episode, you will usually be aware of the rapid beating of your heart.
Other symptoms might include dizziness (blacking out may occur but is unusual), shortness of breath, sweating, chest pain and anxiety. After an episode it is usual to feel very tired.
Is Supraventricular tachycardia dangerous?
In the vast majority of cases SVT is a benign condition. This means that it will not cause sudden death, will not damage the heart or cause a heart attack and will not shorten life expectancy. There are some rare exceptions that will be discussed with you if relevant.
How does Supraventricular tachycardia occur ?
There are 3 main types of SVT. It will not always be obvious which type of SVT you have prior to the electrical study of your heart.
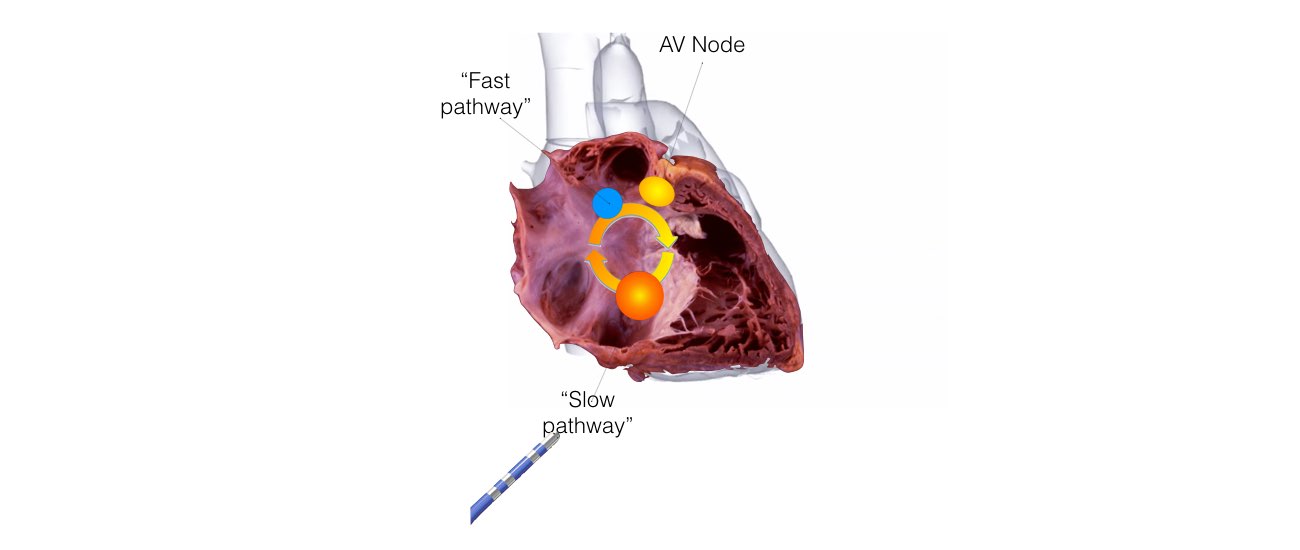
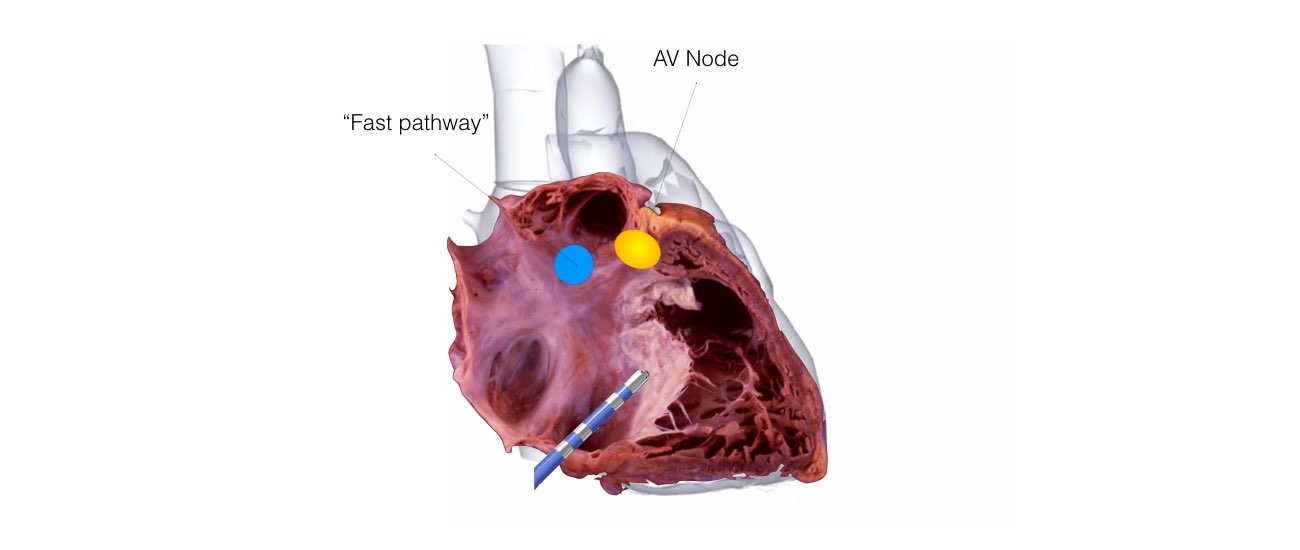
1. AV Nodal Re-entry Tachycardia (AVNRT)
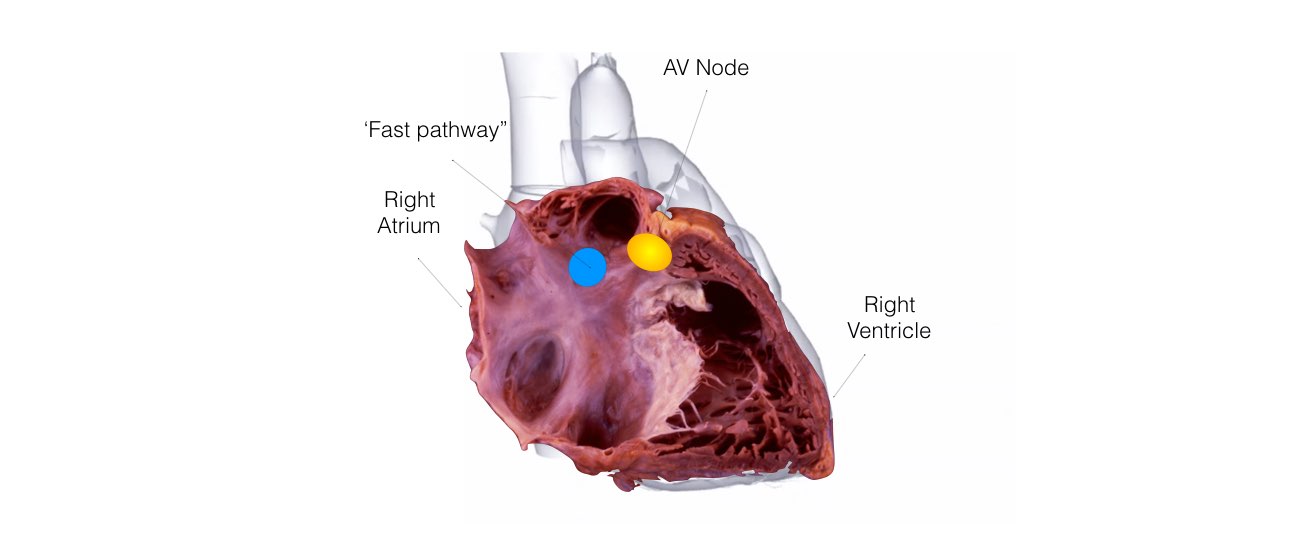
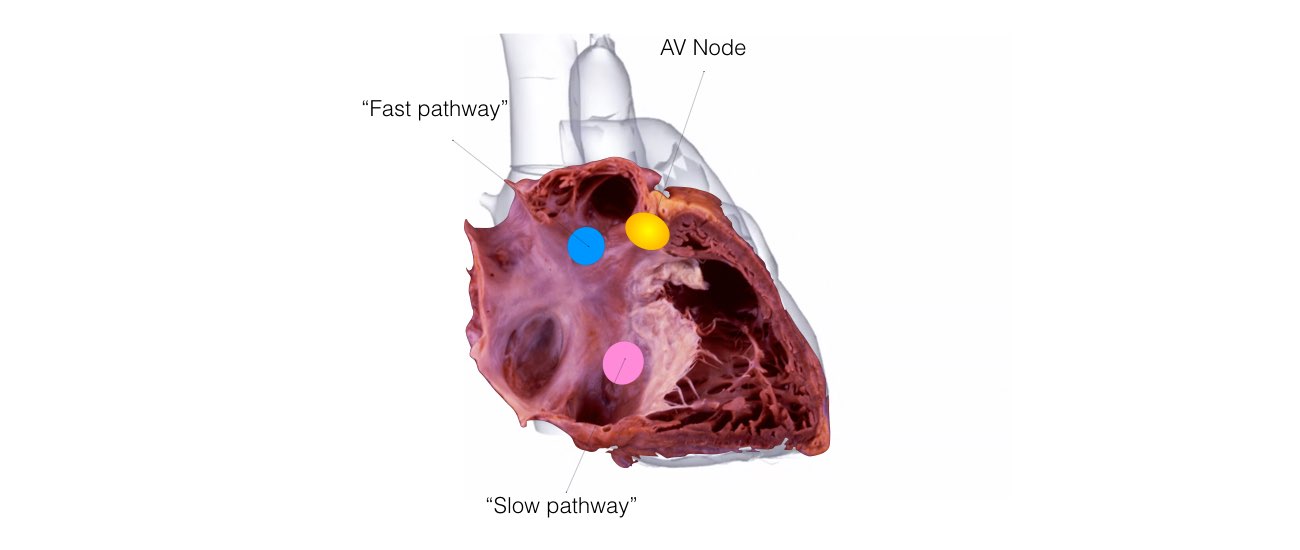
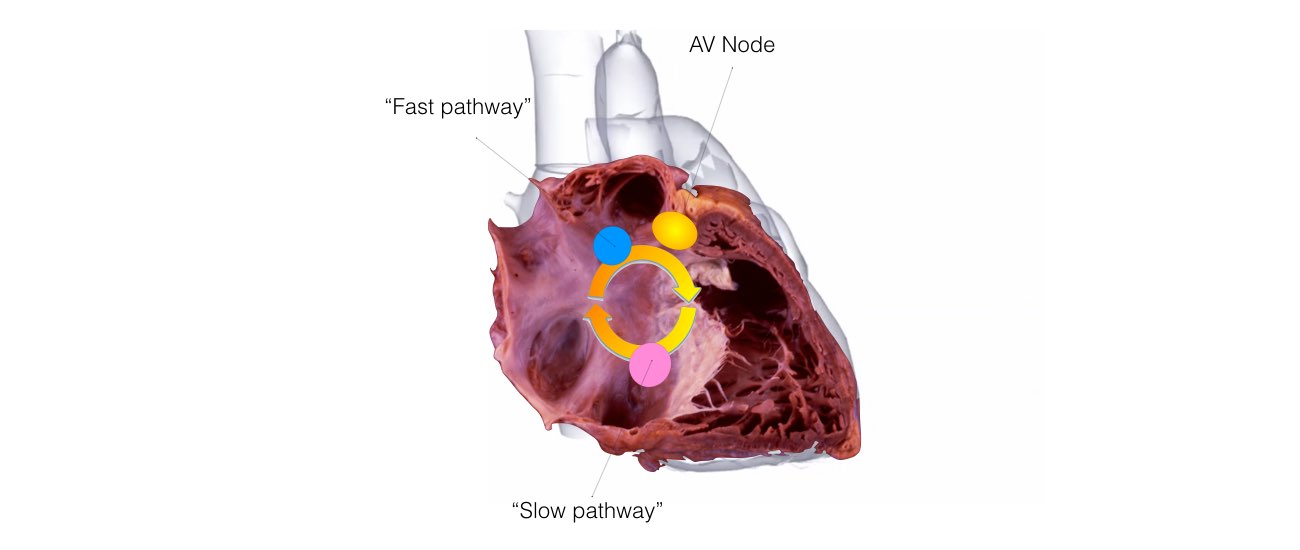
This is the most common form of SVT. An abnormal short circuit (circular conduction) occurs near the AV node. Instead of a single AV node between the top and bottom chambers, there is a second connection that is abnormal. This extra connection has been present since birth. As a result of having 2 connections a short-circuit can occur.
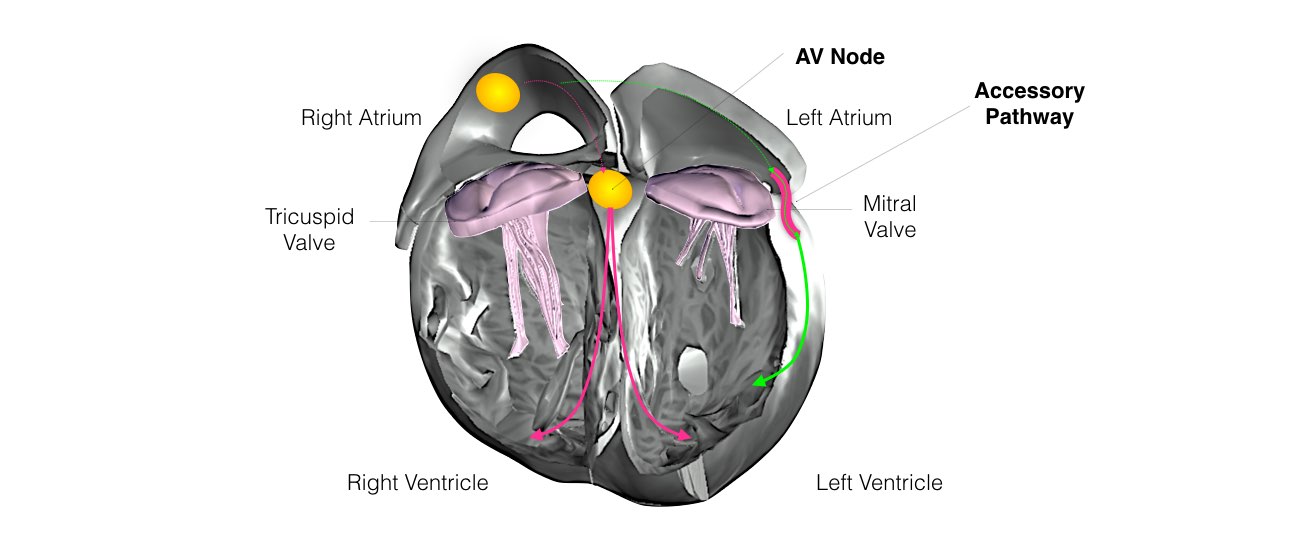
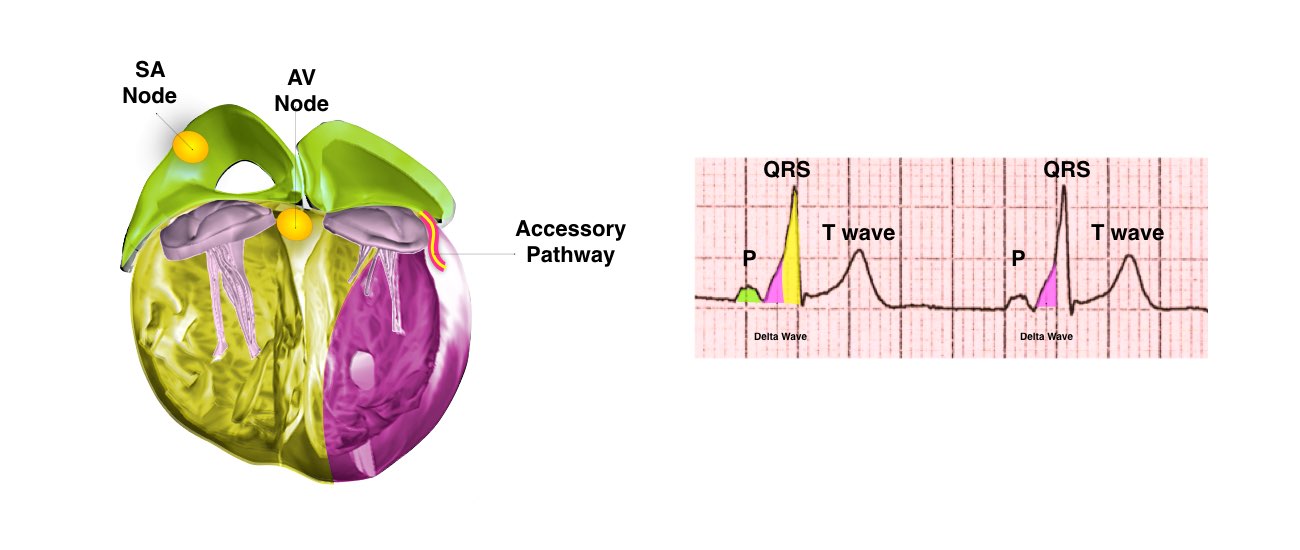
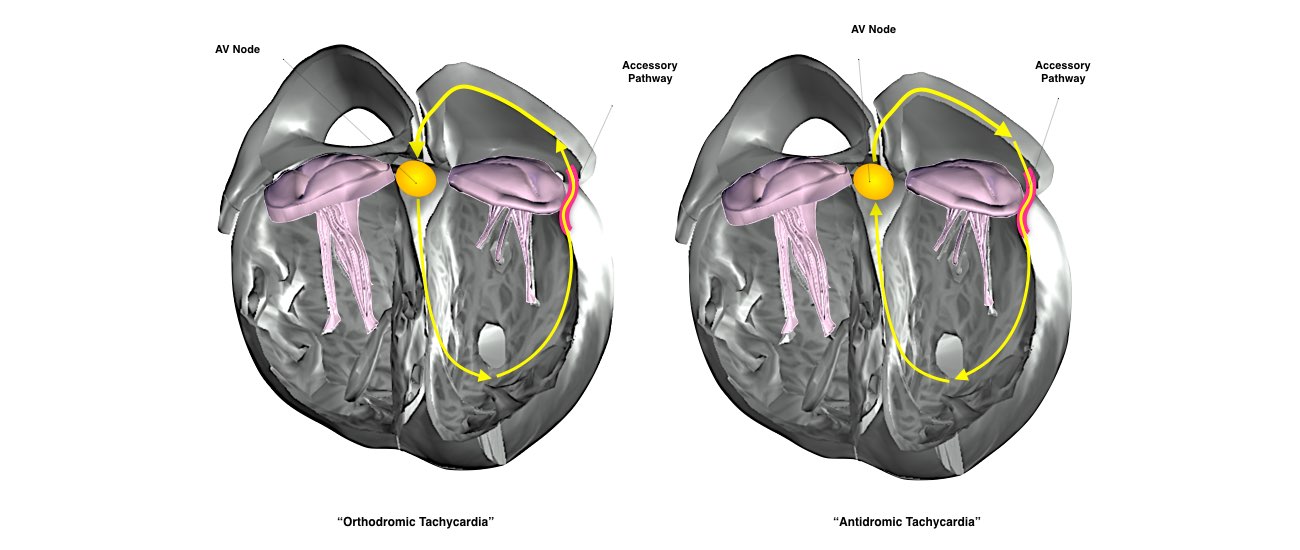
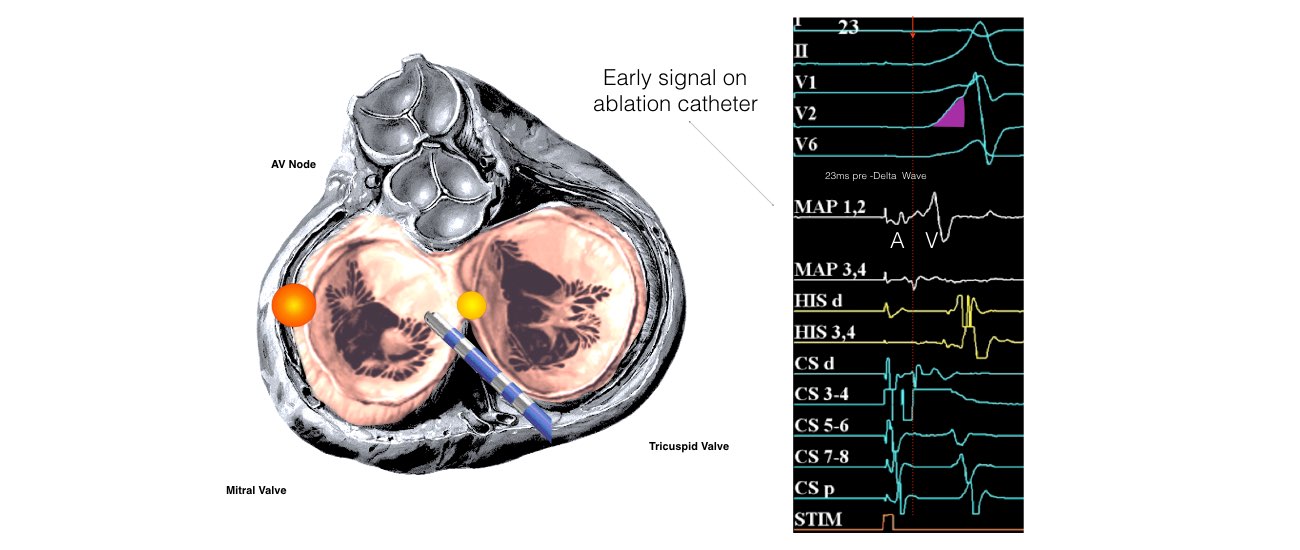
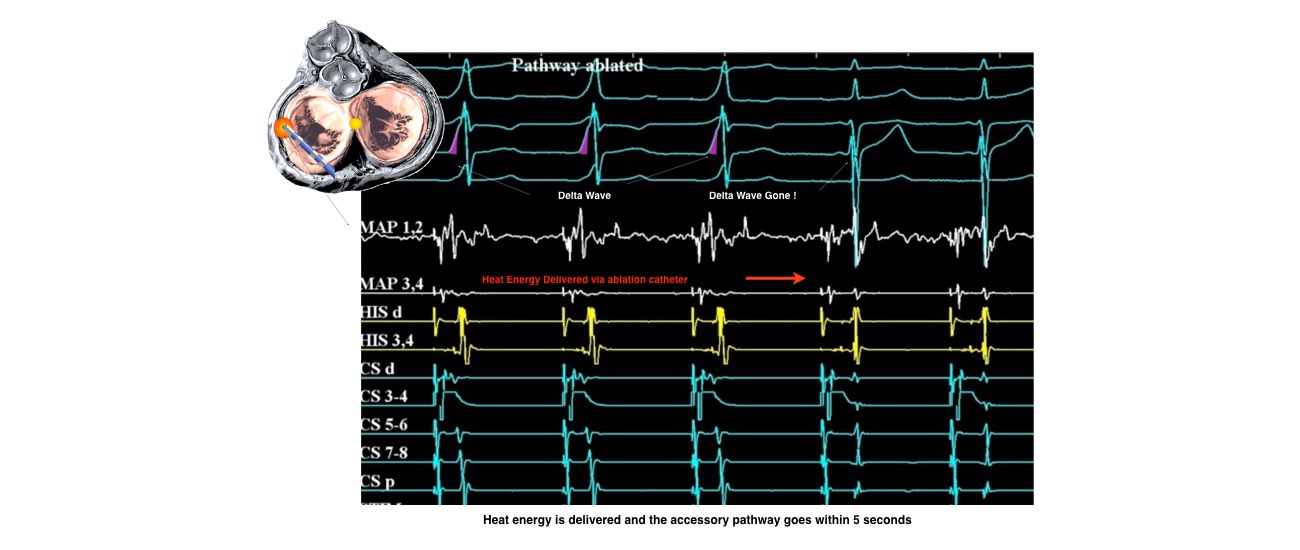
2. Re-entrant Tachycardia and Wolff Parkinson White Syndrome
Abnormal circular conduction utilising the AV node and an “accessory pathway” connecting the atria and ventricles. This extra connection has been present since birth. As a result of having 2 connections a short-circuit can occur. This condition is sometimes termed the Wolff-Parkinson-White Syndrome or WPW.
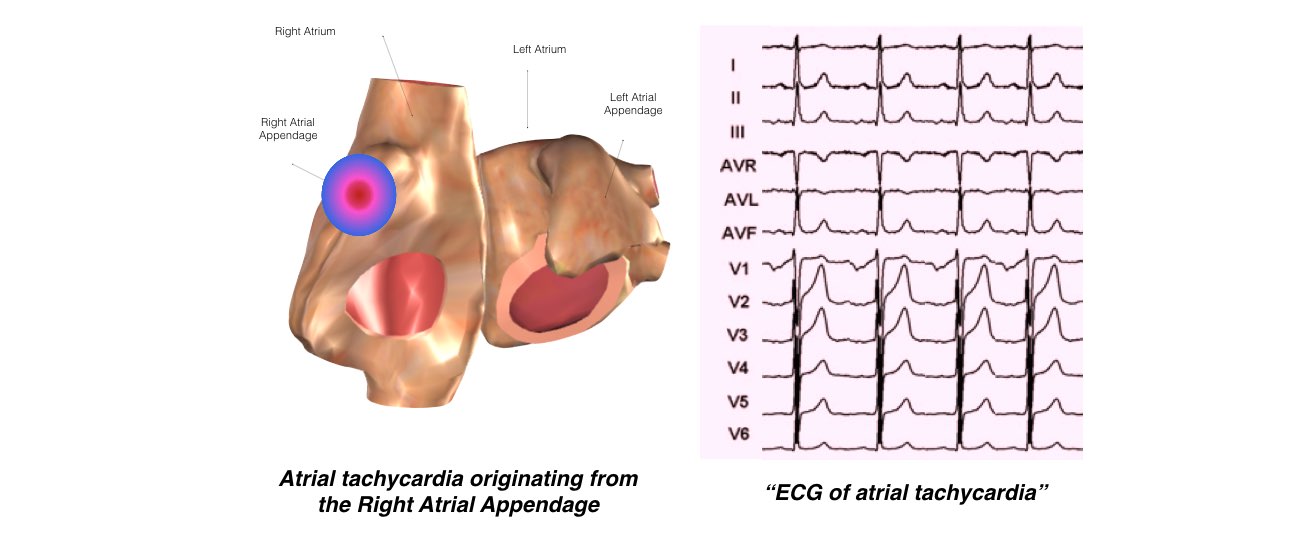
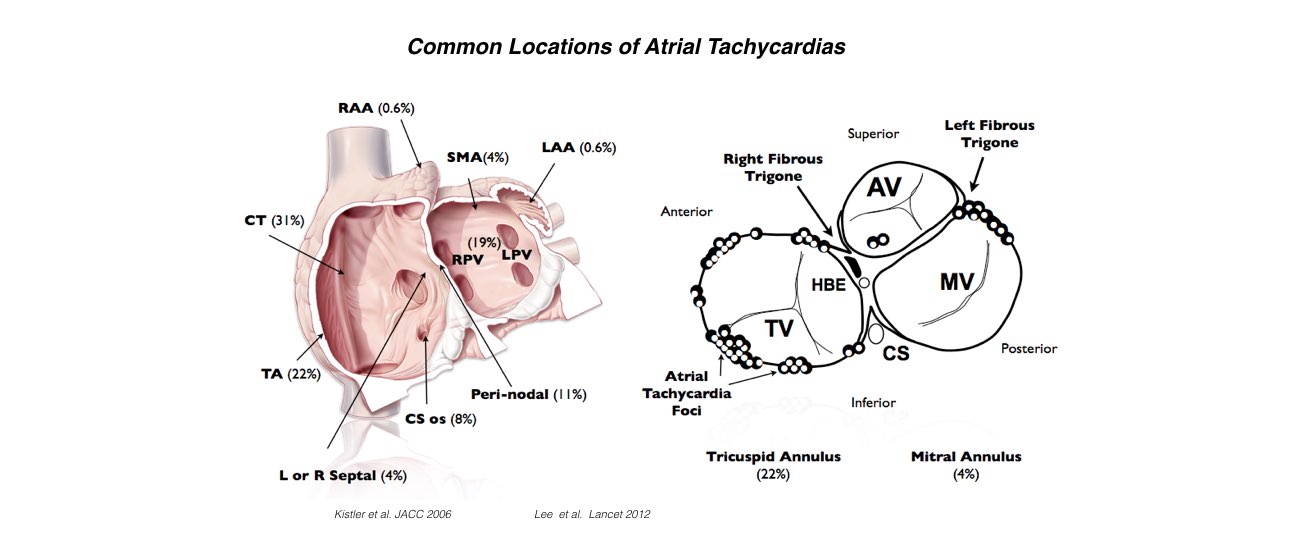
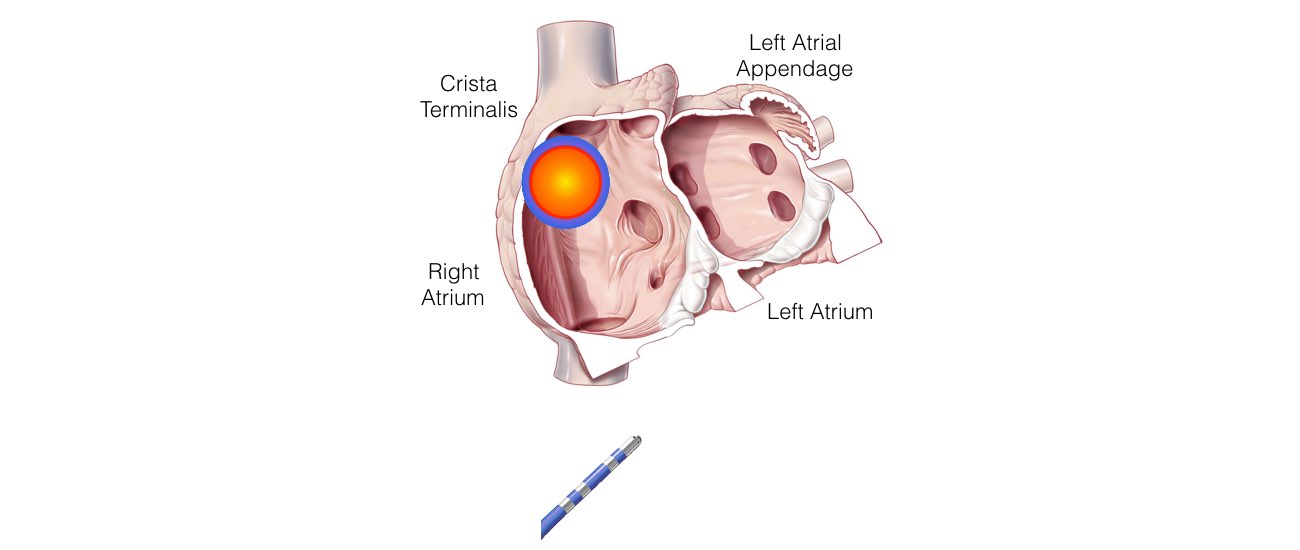
Atrial Tachycardia
This is the least common form of SVT. There is an extra abnormal origin of the electrical impulse from a small area in the atria other than the SA node. It is not known when or why such an extra focus develops