What happens during an Electrical Cardioversion?
The electrical cardioversion is performed in the angiography suite, coronary care unit or recovery room. It is necessary for you to fast for at least 6 hours prior to the cardioversion. You can take your usual medications on the morning of the procedure with a small amount of water. In many cases you will have been on warfarin prior to the cardioversion. It is important that the level of the blood thinning (the INR) is checked prior to the cardioversion, usually the day prior or the morning of the procedure.
Your cardioversion will only be performed if you have had a minimum of 3 weeks whereby your INR has been between 2 and 4. Some patients will be taking the new anticoagulant medications (called NOACs). These are not monitored with the INR so it is important that you tell us if you have not been taking blood-thinning medications regularly for the last 3 weeks.
If you have not been taking your blood thinning medications regularly it is vital that you notify the staff undertaking the cardioversion. Occasionally, a trans-esophageal echocardiogram (TOE) will be performed prior to cardioversion. This is usually done when there is a high index of suspicion of clots inside the heart or your warfarin level has been fluctuating or if you have not taken your NOAC medication regularly.
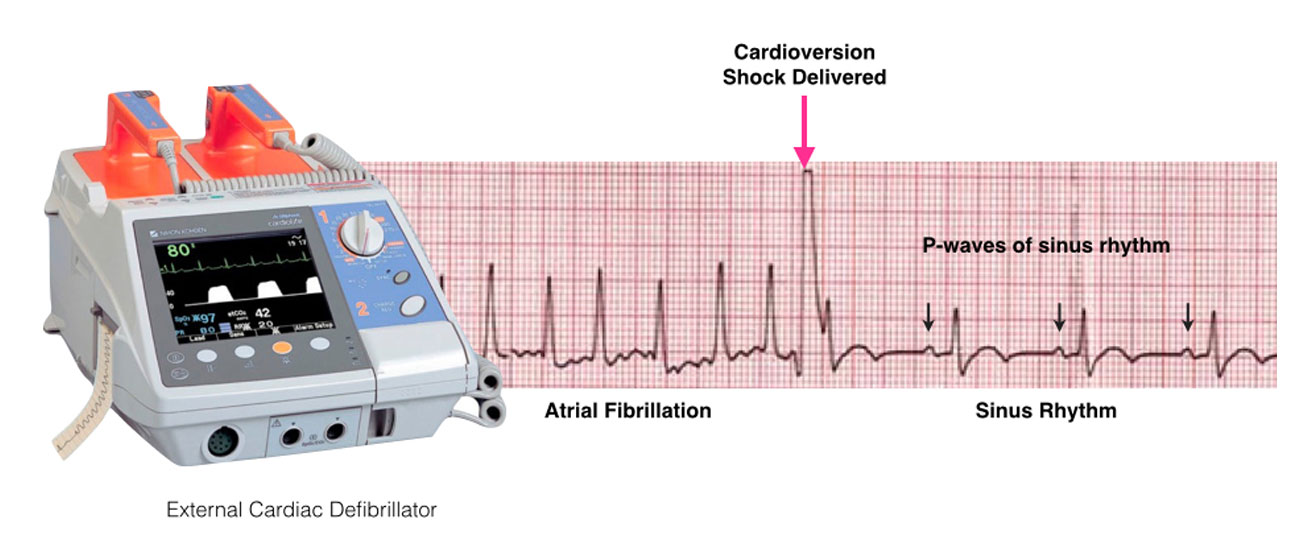
For the cardioversion, special pads are used to minimise any skin burning or irritation from the electrical shock. You will be connected to an external defibrillator to allow monitoring of your heart rhythm and to allow the application of the necessary energy to restore your heart’s rhythm back to normal. As the shock may be uncomfortable, some form of sedation or anesthesia is administered intravenously.
Once you are sedated, the shock is delivered. Additional shocks at higher energy levels can be delivered if the first shock does not restore the rhythm back to normal. The success rate depends upon a number of factors but there is an approximately 90% chance that the normal rhythm (sinus rhythm) will be restored.
There is a very small risk of stroke immediately after the cardioversion procedure as a result of stunning of the top chamber of the heart (atrium). This risk is greatest in the first few weeks after the cardioversion procedure. This is why it is crucial that warfarin is continued (maintaining the INR between 2 and 4) for at least a month after the procedure. For patients on NOACS, it is crucial you take your medications regularly for the next month.
In a proportion of patients, the arrhythmia subsequently recurs and repeated cardioversion may be required. Patients generally wake quickly and without any recollection of the shocks because of the effects of the sedatives.
You will not be able to drive yourself home from the procedure and will need a responsible adult to stay with you overnight after the procedure. You should not drive or make any important decisions for 24 hours after the procedure.
What is a transesophageal echocardiogram?
A transesophageal echocardiogram is a diagnostic test used to view the structures of the beating heart. The procedure is performed under conscious sedation prior to the electrical cardioversion procedure to make sure there are no blood clots in the heart.
In this procedure, a transducer is passed through the mouth and into the esophagus, which lies behind the heart. The transducer sends images of the heart to a monitor. This imaging process is called an echocardiogram. An echocardiogram uses ultrasound waves to create moving pictures of the structures of the heart such as the chambers and valves. In particular we want to make sure there are no blood clots in the heart prior to the cardioversion procedure.