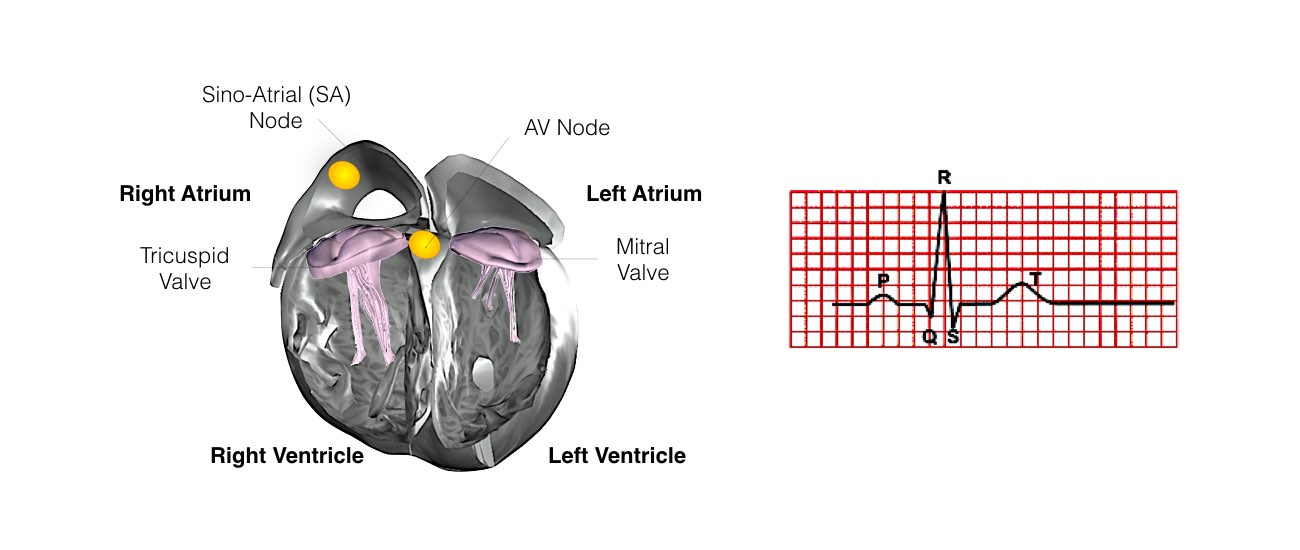
Normal heart rhythm
In order for the heart to do its work (pumping blood throughout the body), it needs a sort of spark plug or electrical impulse to generate a heartbeat. Normally this electrical impulse begins in the upper right chamber of the heart (in the right atrium) in a place called the sino-atrial (SA) node. The SA node is the natural pacemaker of the heart. The SA node gives off electrical impulses to generate a heartbeat in the range of 60 to 100 times per minute. If you are exercising, doing strenuous work or are under stress, your heart rate will be faster. When you rest or sleep your heart rate will slow down. If you take certain medications, your heart rate may be slower.
From the Sinus Node, the electrical impulse is relayed along the heart’s conduction system. It spreads throughout both the right and left atria causing them to contract evenly.
When the impulse spreads over the right atrium it reaches the atrio-ventricular (AV) node. This is a very important structure in the heart because it is the only electrical connection between the top chambers and the bottom chambers. It is therefore the only way in which an electrical impulse can reach the pumping chambers (the ventricles). The impulse spreads through the AV node and down into the lower chambers or ventricles of the heart. This causes them to contract and pump blood to the lungs and body.
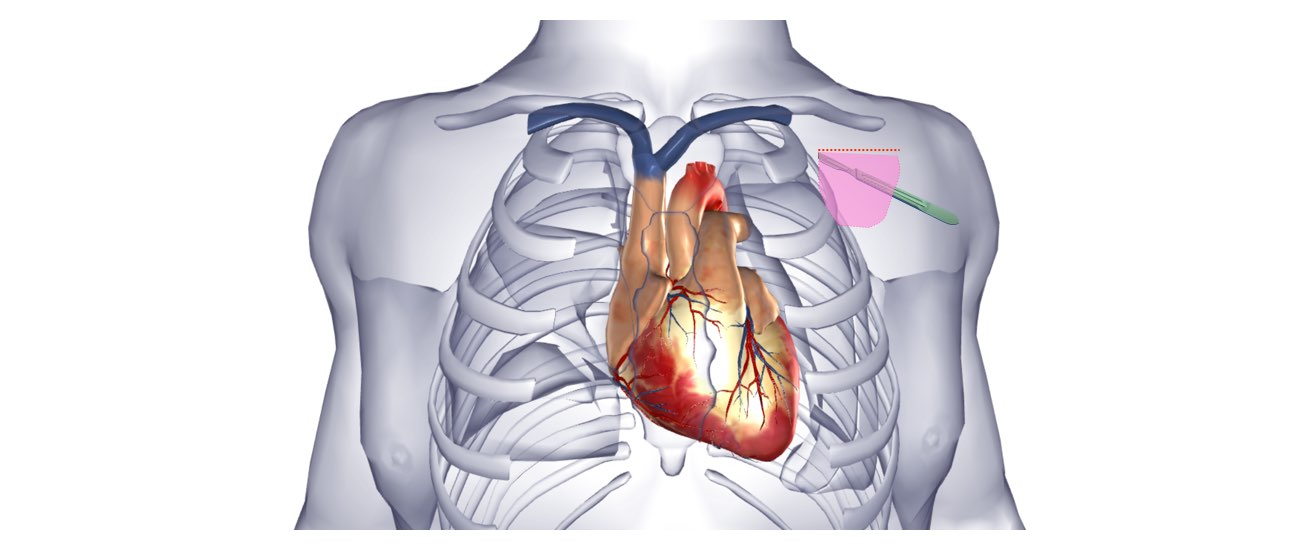
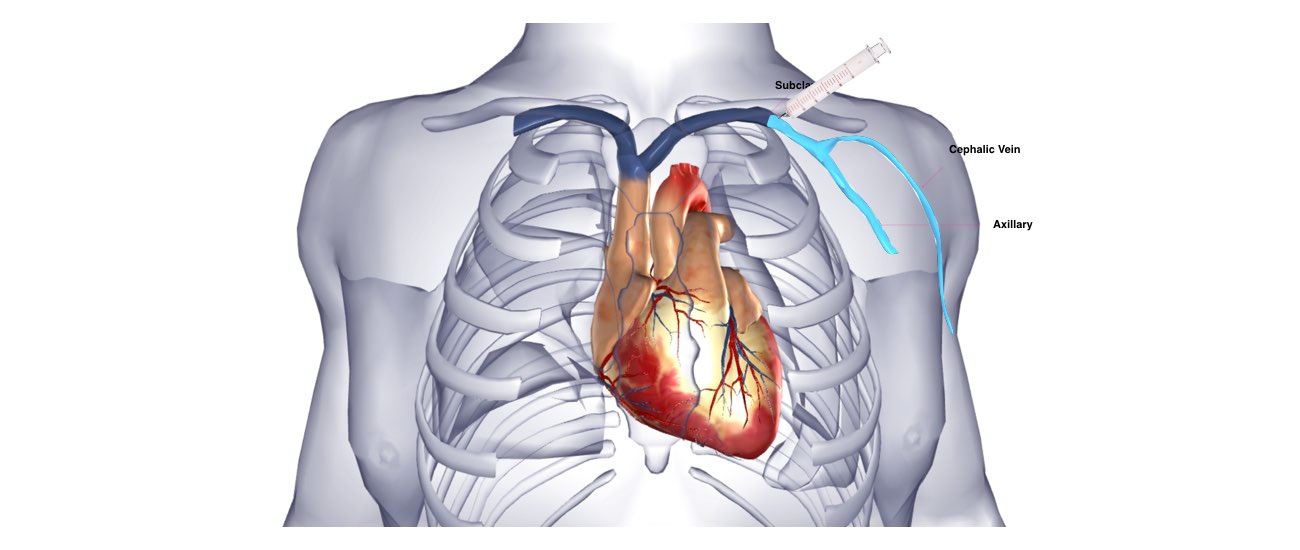
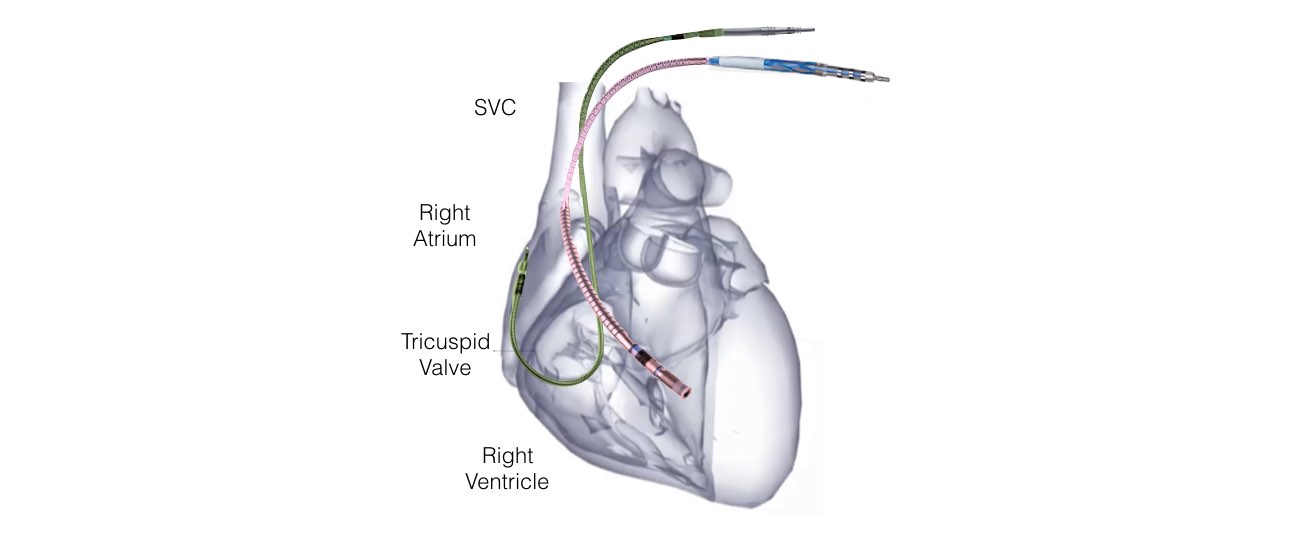
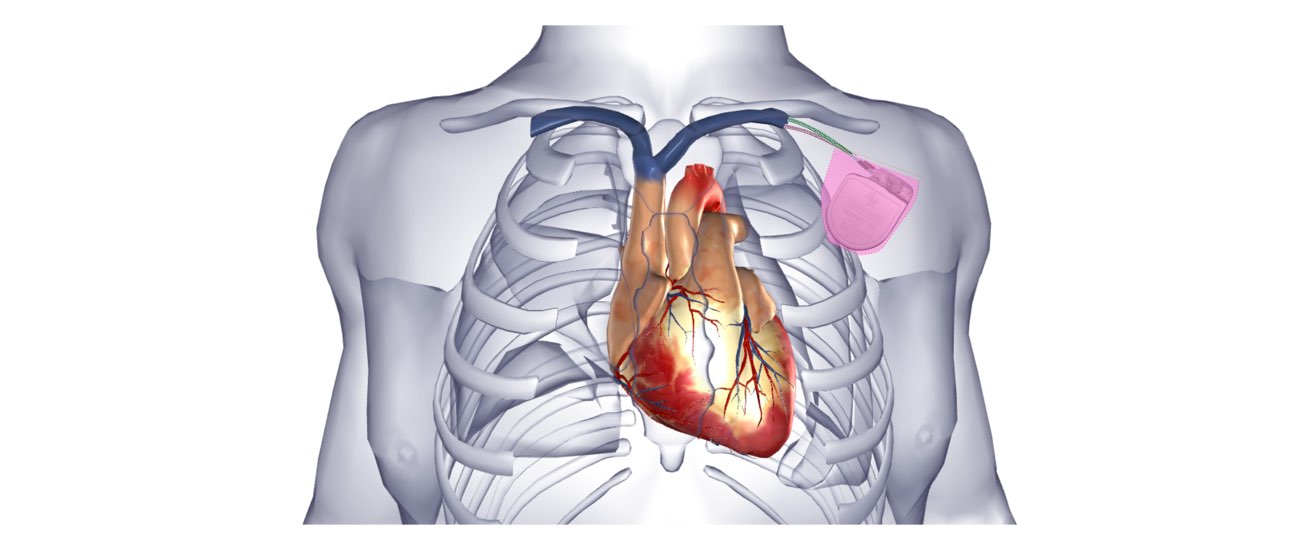
The main body of the device is usually implanted under the skin in your shoulder region. The leads are connected to the device at one end and to your heart at the other end. The leads are able to transfer information about your heart rhythm to the device. The device will determine what rhythm your heart is in and will deliver therapy through the leads when necessary.
Why do I need a defibrillator?
In some people the electrical system of the heart may develop a short circuit in the pumping chambers (ventricles). This short circuit is termed Ventricular tachycardia or ventricular fibrillation. These rhythm disturbances cause the heart to beat too rapidly and inefficiently so that not enough blood is pumped to the brain.
The usually symptoms are intense dizziness, or sudden collapse with loss of consciousness.
These heart rhythm disturbances are potentially fatal.
Your doctor is recommending you have a defibrillator either because you have had one of these rhythm disturbances or because you may be at increased risk of having this in the future.
If the life-threatening rhythm occurs, the defibrillator delivers a high energy shock (up to 750 volts) in order to return the heart to a normal rhythm. This is life-saving treatment.
What is an ICD?
An ICD, or Implantable Cardioverting Defibrillator, is a device implanted in the body that can detect and terminate fast heart rhythms (Ventricular Tachyarrhythmias). An ICD has two main parts”
- Main body (battery and electrical circuitry)
- Leads